GEOMETRIC CONFIGERATION OF CROWN OUTLINE
This blog is to support dental graduates who try to get through mfds/mjds/nbde or ORE...
Pages
▼
Thursday, September 29, 2011
The Etiology of Orthodontic Problems
The Etiology of Orthodontic Problems
Malocclusion and Dentofacial deformities result not only
from some pathological processes, but also by moderate distortions of normal
development.
Tuesday, September 27, 2011
A Note On Etiology, Clinical Features And Management Of Oroantral Fistula
Mx Of Oroantral Fistula
Oro-antral
fistula:
Invasion of the maxillary sinus and establishment of a
direct communication with the oral cavity is referred to as an oro-antral
fistula.
Factors
influencing creation of oro-antral fistula:
Ü Teeth
size and configuration of the roots.
Ü Hypercementosis
and bulbous roots.
Ü Density
of alveolar bone and thickness of sinus floor
Ü Size
of the sinus.
Ü Relation
of sinus to the root of upper teeth.
Ü Rough
extraction and misguided
manipulation.
Ü Apical
pathosis and attached granulomas.
Ü Periodontal
diseases which may erode sinus floor.
Ü Presence
of cysts and neoplasm.
Ü Invasive
surgery e.g. cleft and dental implants placement.
A Video On Buccal Advancement Flap
Monday, September 26, 2011
Sunday, September 25, 2011
A Short Note On Overdentures....with ppt for download.
Overdenture
A complete or partial removable denture supported by retained roots that is intended to provide improved support, stability, and tactile and proprioceptive sensation and to reduce ridge resorption.
Advantages
— Preserve alveolar ridge
— Possibly
-support
-proprioreception
-retention (eventually)
-stress distribution
-support
-proprioreception
-retention (eventually)
-stress distribution
Disadvantages
· Poor oral hygiene
-caries and periodontal disease
— Soft tissue undercuts
-esthetics
-retention
-esthetics
-retention
— Breakage of denture
-thin
-stress concentration over abutments
-thin
-stress concentration over abutments
Selection of abutment teeth
— One per quadrant
— Not adjacent teeth
— Usually mandibular cuspids and premolars
— Maxillary cuspids frequently cause esthetic and retention problems due to soft tissue undercuts
Overdentures
— Regard as transitional
- need perfect oral hygiene
-daily non acidulated topical fluoride (sodium fluoride)
-daily non acidulated topical fluoride (sodium fluoride)
— Probably better to place 2 implants
A Video On Implant Supported OverdentureSaturday, September 24, 2011
A Note on Dental Anatomy of Premolars
General Features of Premolars
Dental Anatomy Lecture Note on Premolars
— They have at least two cusps.
§ one large buccal cusp,
§ Smaller lingual cusp
— The lower second premolar may- sometimes- have two lingual cusps.
Maxillary 1st Premolar
Maxillary 2nd Premolar
Mandibular 1st Premolar
Mandibular 2nd Premolar
OSSEOINTEGRATION IN IMMEDIATE LOADED DENTAL IMPLANTS
IMMEDIATE LOADED DENTAL IMPLANTS
Advantages of immediate placement
1 Implants in fresh extraction sites can be placed in the same position as the extracted tooth, minimizing the need for angled abutments.
2 Osseointegration is more favorable when implants are placed immediate following an extraction.
3 The bony receptors are preserved by preventing atrophy of the alveolar ridge, preventing recession of the mucosal and gingival tissues. Reports indicate that a significant amount of crestal bone is lost by delaying the load on implants.
4 Non-functional restorations can be provided for better esthetics, especially in the anterior region.
5 lmmediate placement of implants keeps contaminants away from the socket.
6 Waiting times for primary healing of the soft tissues and regeneration of the osseous structure are eliminated.
7 More patients will opt for implant treatment (no waiting for healing, immediate restorationA Video Of Dental Implant Procedure
A Note On Nonsteroidal Anti inflammatory Drugs (NSAIDs)
Nonsteroidal Anti inflammatory Drugs (NSAIDs)
Content of Following Presentation Are,—Common adverse effects
—Different pharmacokinetics and potency
—Different chemical families
—Common mechanism of action (cyclooxygenase inhibition)
—Different selectivities to COX I and II
Similarities more striking than Differences
Friday, September 23, 2011
A Lecture Note On Inherited Oral Diseases.......with pdf for download
Inherited Oral Diseases
Disorders Affecting Periodontium/Gingiva
• Papillon-LeFèvre Syndrome
• Cyclic Neutropenia
Disorders affecting Jaw bones and Facies
• Cherubism
• Cleidocranial dysplasia
• Gardner syndrome
• Mandibulofacial dysostosis(Treacher-Collins syndrome)
• Nevoid basal cell carcinoma syndrome
• Osteogenesis Imperfecta
• Aperts Syndrome
• Crouzon Syndrome
Disorders affecting Oral Mucosa
• Hereditary Hemorrhagic Telangiectasia
• Multiple Endocrine Neoplasia Syndrome IIB
• Neurofibromatosis
• Peutz-Jeghers Syndrome
• White Sponge Nevus
Disorders of Teeth
• Amelogenesis Imperfecta
• Dentinogenesis Imperfecta
• Dentin Dysplasia
• Hypohidrotic ectodermal dysplasia
• Hypophophatasia
• Vitamin D deficient rickets
• Autosomal Recessive
• Cathepsin C gene mutation which affects the immune response to infection
• Hyperkeratosis of the palms and feet
• Sometimes elbows and knees
• Dramatic periodontitis (periodontoclasia) of both dentitions
– Floating teeth
– DD: Langerhans’ cell disease
Teeth erupt in normal sequence, position and time
1.5 to 2 years, a severe gingivo-periodontal inflammatory process develops
Edema, bleeding, alveolar bone resorption, and mobility of teeth with consequent exfoliation
Teeth are lost in the sequence they are erupted. After loss of last teeth, gingiva regains a normal appearance
Permanent teeth are lost before 14 years
Peripheral blood neutrophil is depressed in all patients with Papillon-Lefèvre suggesting that neutrophils are important factor in pathogenesis of severe periodontal disease
Treatment
Retinoid therapy: Improves the skin condition but not the periodontal therapy
Periodontal condition: No effective treatment
• Autosomal dominant
• Facial appearance similar to “cherub”-like
• 2 – 5 yrs of age
• The clinical alterations typically progress until puberty, stabilize and slowly regress
• Bilateral involvement of the posterior mandible – most common appearance – “cherub”-like (all 4 quadrants)
• “Eyes upturned to heaven” appearance – due to involvement of the infraorbital rim and orbital floor
• Painless bilateral expansion of the post. mand.
• Marked widening and distortion of alveolar ridges
• Tooth displacement and eruption failure
• Multilocular radiolucency with massive expansion
• Both erupted and unerupted teeth are randomly distributed
• After stabilization, lesions exhibit a “ground glass” appearance
• Similar to giant cell granuloma
• But clinical and radiographic correlation necessary
• Vascular fibrous tissue and giant cells (smaller and more focal)
• Eosinophilic cuffing around blood vessels
Treatment
• Prognosis is unpredictable
• Delayed till after puberty (curettage)
Caused by a defect in Cbfa1/Runx2 gene
Autosomal dominant and sporadic pattern
Bone defects involve the clavicle and skull
Clavicles are absent (unilateral or bilateral) – 10% of cases
Short stature with large heads; ocular hypertelorism; broadbase of nose and depressed nasal bridgebase of nose and depressed nasal bridge
Large heads and parietal bossing
Skull sutures show delayed closure and may remain open
Dental manifestations include narrow, high-arched palate with increased prevalence of cleft palate
Presence of numerous unerupted permanent and supernumery teeth with many distorted crown and root shapes supernumery teeth with many distorted crown and root shapes
Prolonged retention of deciduous teeth and delay or complete failure of eruption of permanent teeth
Histology:
Unerupted permanent teeth lack secondary cementum Unerupted permanent teeth lack secondary cementum
Treatment:
No treatment; full-mouth extractions with denture construction;
removal of primary and supernumery teeth followed by removal by exposure and orthodontic treatment of permanent teeth
Craniosynostosis: Premature closure of sutures
Mutation in FGFR2; 1 in 65,000 births; AD
Wide variation in clinical presentation: Brachycephaly; scaphocephaly; trigonocephaly; “cloverleaf” skull (kleeblattschädel)
Ocular proptosis: blindness and hearing deficit
Headaches; normal intelligence
Underdeveloped maxilla: Midface hypoplasia; crowding of maxillary teeth; bifid uvula
Surgical treatment
Craniosynostosis syndrome
Mutation in FGFR2; 1 in 65,000 to 160,000 births, AD
Acrobrachycephaly (tower skull); kleeblattschädel (severe cases)
Ocular proptosis; hypertelorism; vision loss; “beaten metal”radiographs
Midface hypoplasia; ‘V”-shaped arch “open-mouth” feature; hearing loss
Pseudo cleft palate due to swellings (accumulation of glycos-aminoglycans) of the lateral hard palate and crowding of maxillary teeth; bifid uvula
Surgery
Defects of 1st and 2nd BA
AD; 1 in 25,000 to 50,000 births; 60% new mutations
Mutations in the TCOF1 gene
Characteristic face: Hypoplastic zygoma causing narrow face with depressed cheeks and downward slanting palpebral fissures
Coloboma (notch) at the outer portion of lower eyelid
Ears anomalies: Deformed pinnae, extra ear tags, middle ear ossicle defects cause hearing loss
Underdeveloped mandible; condyle and coronoid hypoplasia
Lateral facial clefting and cleft palate
No treatment required in most cases; Cosmetic surgery in severe cases
• A.D.; 50% of cases are new mutations; 1:3,000 births
• Many forms
• NF1 most common; chr. 17
• Malignant transformation
• Diagnostic criteria (2 or more needed)
– Six or more café au lait macules over 5mm in prepubertal and 15mm in postpubertal
– Two NFs or one plexiform NF
– Axillary freckles (Crowe’s sign)
– Optic glioma
– Lisch nodules (brown pigmented spots of the iris)
– Distinct osseous lesions (thinning of long bone cortex)
–1st degree relative with 2 or more of these findings
• Oral lesions
–NFs anywhere
– Enlargement of fungiform papillae
– Enlargement of mandibular foramen
– Enlargement of the mandibular canal
Download A Note on Inherited Oral Diseases…..pdf
Thursday, September 22, 2011
A Lecture Note On Histopathology Of Dental Caries
- Dental caries or tooth decay is one of the most common of all disorders, second only to common cold.
- Dental caries has afflicted more humans longer than any other disease. It was first appeared about 14000 years ago. From that time to the present, dental caries affected almost all human populations, at all socioeconomic levels, and at all ages.
- The first study about dental caries was published in 1870 and has continued uninterrupted to the present.
- Every year $20 billion is spent in USA for prevention of dental caries.
- Some isolated populations like Eskimos, some African natives, and inhabitants of rural India are “immune” to dental caries because they are not exposed to western food habits.
- The word ‘caries’ is derived from the Latin word ‘rot’.
- In 1982 Dr. Louw calculated that it would take 470 dentists, working all year long , to restore the carious lesions in 12-year old ‘colored’ children in South Africa.
è It is the most prevalent disease affecting the human race,
è Practically spread all over the world,
è Affects both sexes and all races, all socio-economic strata and people of all ages,
è Starts soon after teeth erupt into the oral cavity
è It is a paradox that teeth are the hardest tissue in the body but can be easily destroyed relatively rapidly in vivo.
What is Dental Caries?
It is a microbial disease of the calcified tissues of the teeth, characterized by demineralization of the inorganic portion and destruction of the organic substance of the tooth.
Smooth surface Caries:
Due to plaque formation on enamel. The earliest manifestation of incipient caries (early caries) of enamel is usually seen beneath dental plaque as areas of decalcification (white spots).
The first change seen histologically is the loss of inter-rod substance of enamel with increased prominence of the rods.
-this is followed by the loss of mucopolysaccharides in the organic substance.
-presence of transverse striations of the enamel rods,
- accentuated incremental lines of Retzius
as it goes deeper, the caries forms a triangular pattern or cone shaped lesion with the apex towards DEJ and base towards the tooth surface. Finally there is loss of enamel structure, which gets roughened due to demineralization, and disintegration of enamel prisms.
Read and download Following Note On Histopathology of Dental Caries
Videos On Formation Of Dental Caries
buy or rent now
Wednesday, September 21, 2011
A Note ON Immediate Dentures......With ppt Download
Immediate Dentures
An immediate denture is “a complete denture or removable partial denture fabricated for placement immediately after the removal of natural teeth”
Types
Conventional immediate denture:
the denture is intended to be relined to serve as the long-term prosthesis.
the denture is intended to be relined to serve as the long-term prosthesis.
Interim (or transitional) immediate denture (IID):
after healing is completed, a second, new complete denture is to be fabricated as the long-term prosthesis.
after healing is completed, a second, new complete denture is to be fabricated as the long-term prosthesis.
Advantages
- — Maintenance of a patient's appearance
- Circumoral support, muscle tone, vertical dimension of occlusion, jaw relationship, and face height can be maintained. The tongue will not spread out as a result of tooth loss
- Less postoperative pain is likely to be encountered because the extraction sites are protected
- Easier to duplicate (if desired) the natural tooth shape and position
- Adaptation easier. Speech and mastication are rarely compromised, and nutrition can be maintained
Disadvantages
- Immediate dentures are a more challenging
- The anterior ridge undercut that is caused by the presence of the remaining teeth may interfere with the impression procedures
- The presence of different numbers of remaining teeth in various locations frequently leads to recording incorrectly the centric relation position
- No denture tooth try-in in precludes knowing what the denture will actually look like on the day of insertion
- More chair time, additional appointments, and therefore increased costs
A Lecture Note On Immediate Dentures
Lecture note on Anatomy of Salivary glands
The parotid gland
This is the largest of the salivary glands,
lying wedged between the mandible and sternocleidomastoid and overflowing both these bounding structures.
The parotid and its surrounds in a schematic horizontal section—the facial nerve is the most superficial of the structures traversing the gland.
Relations
Above—lie the external auditory meatus and temporomandibular joint.
Below—it overflows the posterior belly of digastric.
Anteriorly—it overflows the mandible with the overlying masseter.
Medially —lies the styloid process and its muscles separating the parotid from the internal jugular vein, internal carotid artery, last four cranial nerves and the lateral wall of the pharynx.
The gland itself is enclosed in a split in the investing fascia, lying both on and below which are the parotid lymph nodes.
Antero-inferiorly, this parotid fascia is thickened and is the only structure separating the parotid from the submandibular gland (the stylomandibular ligament).
Traversing the gland (from without in) are
1. the facial nerve;
2. the retromandibular (posterior facial) vein, formed by the junction of the superficial temporal and maxillary veins.
3. the external carotid artery, dividing at the neck of the mandible into its superficial temporal and maxillary terminal branches
The parotid duct (of Stensen)
The parotid duct (of Stensen) is 2in (5cm) long.
It arises from the anterior part of the gland,
runs over the masseters a finger’s breadth below the zygomatic arch to pierce the buccinator and
open opposite the second upper molar tooth.
The duct can easily be felt by a finger rolled over the masseter if this muscle is tensedby clenching the teeth.
THE RELATIONS OF THE FACIAL NERVE TO THE PAROTID
• The facial nerve is unique in traversing the substance of a gland, a fact of considerable importance .
• This coexistence is explained embryologically; the parotid gland develops in the crotch formed by the two major branches of the facial nerve.
• As the gland enlarges it overlaps these nerve trunks, the superficial and deep parts fuse and the nerve comes to lie buried within the gland.
• The facial nerve emerges from the stylomastoid foramen, winds laterally to the styloid process and can then be exposed in the inverted V between the bony part of the external auditory meatus and the mastoid process.
• This has a useful surface marking, the intertragic notch of the ear, which is situated directly over the facial nerve.
• Just beyond this point the nerve dives into the posterior aspect of the parotid gland and bifurcates almost immediately into its two main divisions (occasionally it divides before entering the gland).
• The upper division divides into temporal and zygomatic branches;
• the lower division gives the buccal, mandibular and cervical branches.
• These two divisions may remain completely separate within the parotid, may form a plexus of intermingling connections,
• The branches of the nerve then emerge on the anterior aspect of the parotid to lie on the masseter, thence to pass to the muscles of the face.
• No branches emerge from the superficial aspect of the gland,
Tuesday, September 20, 2011
A Lecture Note On Bones Of Head........Download ppt
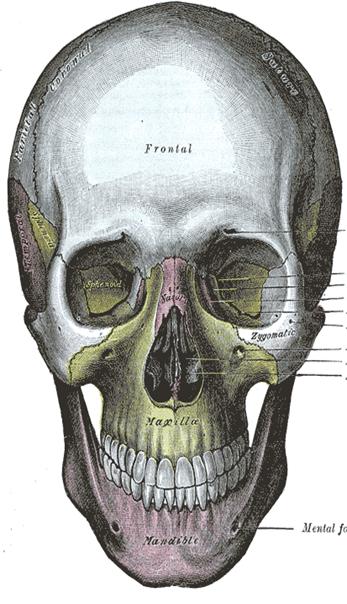
Human skull
The skull is divided into the cranium (all the skull bones except the mandible) and the mandible (or jawbone). One feature that distinguishes mammals and non-mammals is that there are also three ear bones (called ossicles):
- — malleus (hammer)
- — incus (anvil)
- stapes (stirrup)
Maxilla
à is a fusion of two bones along the palatal fissure that form the upper jaw. This is similar to the mandible, which is also a fusion of two halves at the mental symphysis.
Function
—The alveolar process of the maxilla holds the upper teeth, and is referred to as the maxillary arch. The maxilla attaches laterally to the zygomatic bones (cheek bones).
—The maxilla assists in forming the boundaries of three cavities:
— the roof of the mouth
— the floor and lateral wall of the nasal antrum
— the floor of the orbit
The maxilla also enters into the formation of two fossae: the infratemporal and pterygopalatine, and two fissures, the inferior orbital and pterygomaxillaryMandible
A.) Body a.) Symphysis menti
b.) Mental protuberance
c.) Mental foramen
d.) Mylohyoid line
B.) Ramus
a.) Mandibular foramen
b.) Mylohyoid groove
c.) Mandibular canal
d.) Angle
e.) Coronoid process
f.) Condyloid process
g.) Mandibular notch
3D Video Explanation Of Skull Bones