Oral epithelium
Squamous
cell carcinoma
Basal cell
carcinoma
Malignant
melanoma
Salivary glands
Benign
Malignant
Muscles
Bone
Metastatic tumours
Nerves
Blood Vessels, Lymphatics
Multidisciplinary approach in the management
OMF
Surgeon
Oncologist
Pathologist
Anaesthetist
Prosthodontist
Psychologist
Nursing staff
Cancer care workers
Others
Available treatments
1.Curative treatment
2.Paliative treatment
3.Terminal care
Curative treatments
Surgical
treatment
Radiotherapy
(curative,Adjuvant,Neo adjuvant)
Chemotherapy
Chemo prevention
Chemotherapy
Combination
Gene
therapy
Photo
sensitisation
Pre operative care
Investigations
General medical condition:
Hematological- FBC (Hb,PCV),
Clotting profile…
Bio chemical- Liver function, BU,
SC, SE, FBS, UFR
CXR, ECG, 2D ECHO….
Primary lesion:
Adjuncts to biopsy- methelene blue, Vel scope
FNAC, Biopsy, EUA
Endoscopy
Plain x-rays, CT, MRI, PET, Frozen
section
Regional extension: Neck
USS, USS guided FNAC, sentinel node
Bx, CT,MRI
Distant metastasis:
CXR,
USS abdomen, Liver function, Brain CT, Bone scan
Donor site:
X rays, Doppler, Alan’s test.
Patient preparation
Consent
Appropriate referrals
Nutrition
Drugs: warfarin, Heparin, Anti
hypertensives, diabetic drugs….
General hygiene
Oral hygiene
Withdrawal syndrome
Orientation
Plates
Blood
Shaving
Avoid pricking on
donor sites
Allen’s test
Doppler study
Surgical plates / obturators
Antibiotics
Surgical treatment
Surgical treatment
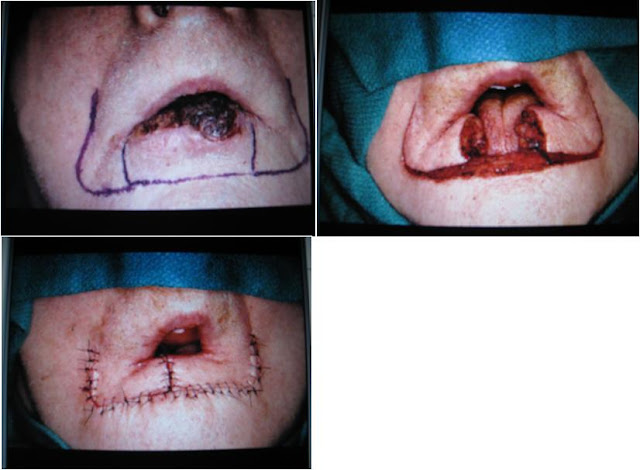
Excision
of primary tumour
Neck
dissection
Reconstruction
Rehabilitation
Social
Physical
Psychological
Follow
up
Primary tumour resection
cheek resection(buccal
mucosa only or full thickness)
mandibulectomy (alveolectomy, segmental, hemi)
Tongue- partial, hemi, subtotal
Maxillectomy
Local
flaps
Random
---- Advancement---Burrows ▲,VY,transpo
---- Pivot
principle---rotational,transposion
Axial ---- fore head, naso labial
Distant
flaps
Deltopectoral
PMMC
Latisimus
Dorsi
Sternomastoid
Trapezius
Free
flaps: RFFF, FFF, LD, R.ab, lat th
Anesthetic considerations
Temperature
Pain
control
Blood
pressure
Hb
Primary and secondary ischemic time
Postoperative Care
01. Postoperative
nursing care:
Trained nurse-1st 24-48
hrs, sterile suction,humidification, rescue stitch-facilitate tube replacement,
slate/pad,pen.
02. Fixation
of the tracheostomy tube:
Dif if dislodged within 48hrs, stitch
to skin. Tapes are enough for 2nd tube, put on neutral position,
knots one each side of the neck (1/3,2/3), should not tight-lymphatic obs,
donot put across the pedicle.
03. Removal
of secretions:
Excess secretions are inevitable,
tube act as f.body,exposed to cold, dry air. Oozing blood. Suck every 30min,
4hrly-immediate post opp period.
04. Humidification:
Warming, humidification-prevent
crusting of secretions. Hot water humidifiers, nebulizers through masks or T
tube to trachy tube. Instillation of saline into the trachea.
05. Changing
of tracheostomy tube:
1st 48 hrs – cuffed tube,
mandatory to use t.tube with inner & outer tubes, this facilitates cleaning
The 1st two changes in
after 48hrs, slightly smaller tube can be inserted.
Thereafter twice a week to avoid
infection & crusting.
Ask the pt to breath in & out,
ask him to hold the breath in expiration (maximum diameter), then insert a
tube.
Within 48hrs, insert a catheter in to
the old tube as guide. Tracheal dilators, laryngoscope. Doctor should be
present at 1st tube change.
06. Care
of the inflatable cuff:
If its pressure exceeds the systolic
blood pressure-ischemic necrosis.
Cuff should be inflated for the 1st
12 hrs following surgery & during this time deflated for 5min every hour.
After 12-24 hr if there is no bleeding,
or not ventilated, let down.
New high volume, low pressure cuffs
are now available.
07. Breathing
exercises:
Physiotherapist,
Is secretions are excessive, vigorous
treatment by intermittent positive pressure breathing or inflated Ambu bag after
suction has been performed.
Block for 24 hrs. if no
difficulties-can be withdrawn. Wound dressings.
08. Dressings:
Changing regularly.
09. Drains:
Vacume should be maintained.
10. Leaking
drains:
Saliva, air or infected secretions
are accumulated underneath the skin flap.
Infection and wound breakdown.
Local packing with saline soaked
swabs or jelonet rolls.
If exit hole is there-pursestring
suture, push the tube in??, Opsite spray,adhessives to cover the hole.
11. Type
of drainage:
After a radical ND:- within 1st
24-48hrs entirely blood appro 200ml/day.
After 48-72hrs become serous,
After 4 days – usually only 25 ml in
24 hrs.
If a localized fistula occur pack
& allow to heal by 2ry intention.
Presence of chyle or lymphatic leak
within the d.tube. ????
12. Removal
of drains:
Remove when it stops draining?????
If there is a problem-blockage-remove
it-otherwise infection.
Should not be removed until the
drainage is less than 25ml, colour become blood red to serum.
Sucking serum from capillaries.
Remove by the 4th or 5th
day if the daily drainage has been consistent for 48hrs.
13. Intravenous
fluid:
Head & neck Sx pts: NG tube, PEG,
open gastrostomy or Jejunostomy. Usually not require parental feeds, can fed
within 48hrs of operation.
In 1st 48hrs pt must not
given too much water & salts----pulmonary oedema.
Between the end of operation &
next day morning---IV fluids (responsibility of the anesthetist & surgical
team).
Blood & fluids if required.
Through CVP line.
CVP can be removed if the pt – if Hb
& electrolytes are normal, NG tolerating, CVP is not needed for any other
solutions or antibiotics.
Urinary output ? Early hrs, fluid
balance??
14. Oral
feeding:
In major abdominal Sx-after GIT
function.
H&N sx – can be given if bowel
sounds have returned.
Can be fed from day 1.
NG tube, PEG, open gastrostomy or Jejunostomy
where enteral feeding is anticipated for short period after Sx.
For longer periods-Preopp PEG under
LA with sedation. PEG is helpful if the pt need post opp RT.
Full strength feeds providing about
2400 kcal in 24 hrs can be achieved on the 2nd day.
Pts who do not have above methods-IV
nutrition (parental nutrition-TPN) for several day after sx. Cost???
Sepsis ???
15. DVT
prophylaxis:
Pt assessment for high, moderate
& low risk.
Low risk pts – mobilize early.
Moderate risk pts – early mobi,
TED-graduated compression stokings.
High risk pts – including all H&N
oncology pts – perioperative & post operative Sc LMW heparin (Tinzaparin
3500 units daily), until the pt mobile, along with TED.
16.
Monitoring of flaps:
Local flaps:- require observation,
distant pedicled flaps-observe for 1 week. (gross vascular changes…), revision
may required.
MV free flaps:- constant monitoring,
often go wrong in the 1st 48 hrs
Medications:
Antibiotics:
Prophylactic AB cover is indicated in
a number of situations.
It is not required for clean
Sx-superfi,parotidectomy, MRND. Last for < 3hrs.
Longer procedures, shaving-within
24hrs: short AB prophylactic cover (48hrs)
Co-amoxiclav or Cefuroxime.
Specific indications: anti MRSA therapy.
Main indication for prophylactic AB
in H&N sx for-mouth pharynx,larynx, upper oesophagus.
Gram +ve cocci & anaerobes.
Gram –ve cocci- seldom present,
colonize the mouth within 2-3 days.
Co-amoxiclav or Cefuroxime and
Metronidazole.
Erythromycin – significant GIT upset,
not tolerated IV.
If risk of post opp infection
continue for 5 days.
If infected – swabs, culture & ABST.
Chest infection should be prevented.
Oral hygiene – important.
Thyroid & parathyroid
replacement:
After total thyroidectomy,
parathyroidectomy—Ca balance, thyroid hormone repla
Half life of thyroxine is 10 days,
can start 1 week after the sx. Thyroxine 100ug/day, in elderly 50ug/day.
On discharge 150ug/day
Dressings &
Sutures:
Wound dressings- several ADR;
Make the wound warm
Macerated & liable to infection
Haematomas?
Small amount of gauze dressing to
prevent small leak. Removed after 12-24 hrs.
Not a good idea to apply pressure
bandages around the neck;
Occlude venous return via vertebral
veins.
But
has a value after parotidectomy for 24hrs-prevent haematoma.
Sutures:
Skin sutures can be removed in 7 days,
Extend to 10 days if he received
previous RT,
After laryngectomy 10 days to 2 weeks:
tension, dif to remove with laryngectomy tube,
Monofilaments synthetic sutures can
be left longer than silk,
(silk-micro abscesses within 72 hrs),
Intra oral Vicryl do not need to be removed.
Post operative examination:
Twice a day:- H&N, chest, abdomen
and calves.
Getting up:
As soon as possible after Sx,pt can
propped up in bed at 45 degree to avoid lymphatic stasis.
Bilateral ND-never lie flat. Danger
of cerebral oedema.
After carotid blow out pt must be
nurse flat for 48hrs. Then raise by 1 pillow per day.
Pt should be walking freely around
the ward within 72 hrs. helps to prevent post op chest infection & DVT.
Follow up:
risk of developing recurrent disease,
Should be followed up at regular
intervals,
In each follow up visit-examine;
Primary site for recurrence
Neck for LN














Looking for Dentist in Mesa,AZ? Click to learn why we are best dental implant provider. Dental implants are a beautiful, permanent solution to missing teeth! Call us today! We serve patients all over in Mesa.
ReplyDeleteI was diagnosed as HEPATITIS B carrier in 2013 with fibrosis of the
ReplyDeleteliver already present. I started on antiviral medications which
reduced the viral load initially. After a couple of years the virus
became resistant. I started on HEPATITIS B Herbal treatment from
ULTIMATE LIFE CLINIC (www.ultimatelifeclinic.com) in March, 2020. Their
treatment totally reversed the virus. I did another blood test after
the 6 months long treatment and tested negative to the virus. Amazing
treatment! This treatment is a breakthrough for all HBV carriers.
I've been living with Parkinson’s for several years. When my usual medications started losing their effectiveness, I decided to explore alternative options. I came across a natural approach from NaturePath Herbal Clinic. Honestly, I was skeptical at first — but after about four months on their herbal program, I started to notice meaningful changes: reduced tremors, less muscle stiffness, and better sleep quality.
ReplyDeleteIt’s not a cure, but for me, it’s been a noticeable improvement in daily life. If you're considering natural or complementary options alongside traditional treatment, this might be something worth checking out: www.naturepathherbalclinic.com.