Radiographic Anatomy of Facial Bones
 |
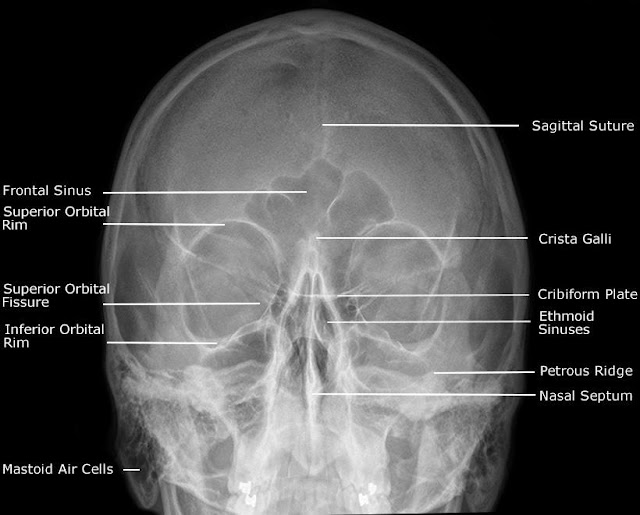
Postero-Anterior Caldwell View
|
 |
Occipito Mental (OM) (Waters) View
|
 |
Postero-Anterior 30° (Modified Parietocanthial)
|
 |
Occipito Mental 30° (OM30) View
|
 |
Submentovertex (SMV) / Slit Basal / Jughandles View
|
 |
Adult Facial Bones - Lateral View
|
 |
Slit Townes View
|
|
Abnormalities
of the Skull and Facial Bones
|
|
|
Cause
|
Radiological Features
|
|
Enlargement of Skull Vault
|
|
|
Children
|
|
|
Hydrocephalus
|
Sutural
diastasis, increased convoluted
markings, “copper beaten skull”
|
|
Raised intra cranial pressure
|
Bulging of fontanelle in infancy.
|
|
Adults
|
|
|
Acromegaly
|
Enlarged frontal sinuses and mandible, erosion
and enlargement of sella turcica
|
|
Paget’s disease
|
Thickened skull vault, increased density of vault
and facial bones.
|
|
Increased
Density
|
|
|
Localised
|
|
|
Hyperostosis frontalis
|
Symmetrical thickening of the inner table of
skull vault, usually in women, of no significance.
|
|
Meningioma
|
Area of
localised sclerosis, possible enlarged
groove of feeding artery.
|
|
Fibrous displasia
|
Asymmetrical, affecting the facial bones maxilla
and base of skull.
|
|
Generalised
|
|
|
Paget’s disease
|
Irregular sclerosis with thickened vault.
|
|
Secondary deposits. e.g. prostate & breast
|
Irregular sclerosis, thickened vault.
|
|
Lytic
lesions
|
|
|
Childhood
|
|
|
Secondary deposits, neuroblastoma, leukaemi
|
Variable appearances, Sutural deposits may
mimic sutural diastasis.
|
|
Eosinic granuloma, Histiocytosis X
|
Transradient defect with bevelled edges.
|
|
Adults
|
|
|
Myelomatosis
|
Rounded translucent (2-10mm) multiple ‘holes’
|
|
Secondary deposits
|
Generally ill defined translucent patches.
|
|
Hyperparathyroidism
|
Mottled appearance of ‘pepper pot’ skull.
|
|
Paget’s
|
Sharply defined zones affecting large areas of
the vault.
|
Radiographic Anatomy of Mandible
 |
Mandible - Postero-Anterior View
|
 |
Mandible - Oblique View
|
 |
Mandible – Lateral View
|
 |
Orthopantogram (OPG)
|







